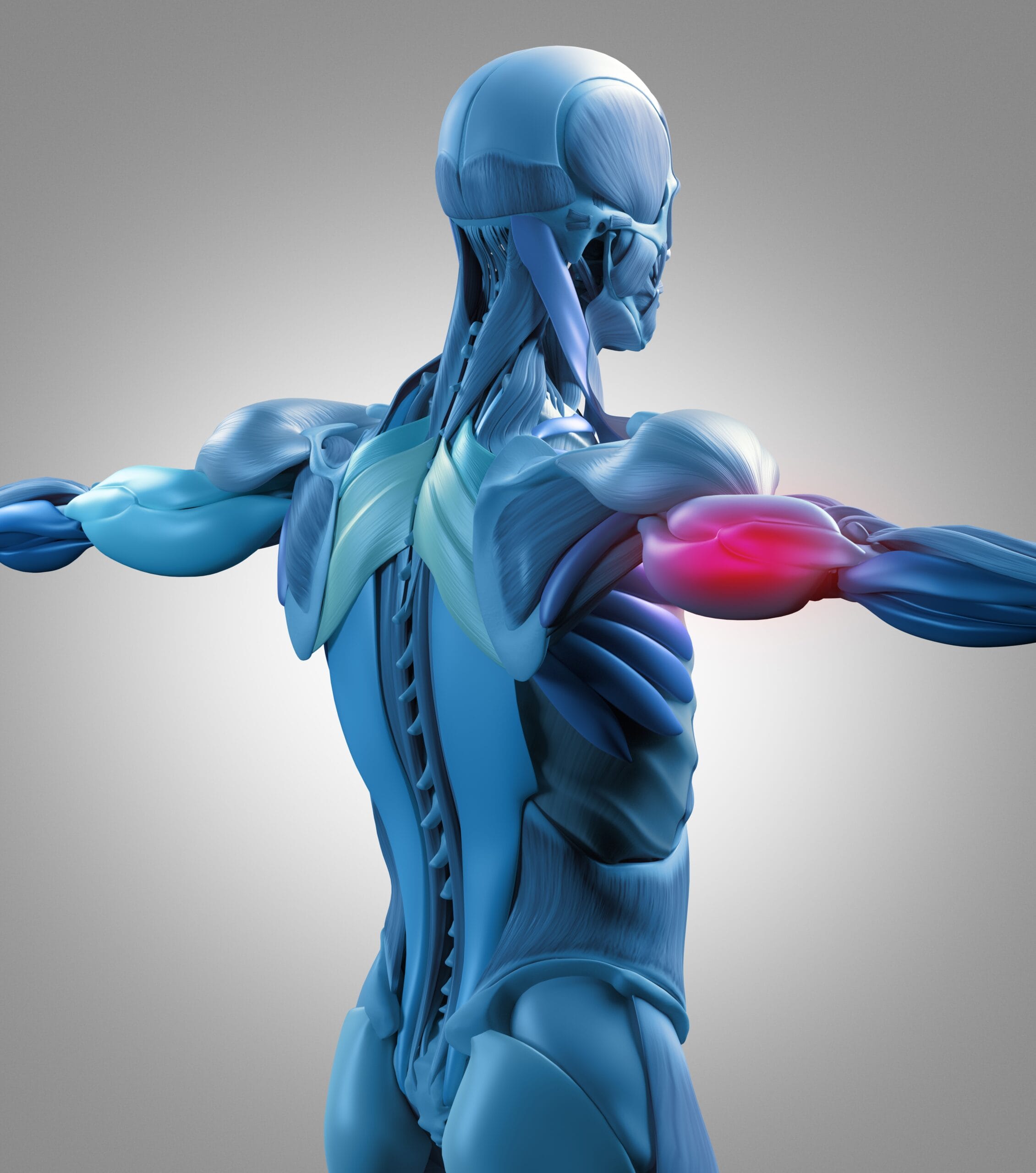
Combat Arts Wrist Injuries Overview
The wrist is one of the most commonly injured areas for martial artists. Damage to any part of the wrist can cause pain and affect the ability to use wrists and hands. Combat sports such as BJJ, karate, tae kwon do, and MMA have the most injuries involving the wrists and hands.

The wrist is composed of eight bones, called the carpals, connected into two rows by ligaments. This arrangement gives the wrist its suppleness, strength, and ability for fluid movement.
These bones are vulnerable to damage from too much pressure such as during a fall or wrist lock which may permanently cripple the wrist or hand. A great resource to own for any martial artist, trainer, or coach for diagnosing and treating wrist and hand injuries is Hand and Wrist Injuries in Combat Sports: A Guide to Diagnosis and Treatment, by Luchetti, Pegoli, et al.
It is not uncommon to hear that a martial artist broke their wrist. Jet Li broke his right wrist while filming The Master. It took some expert fight choreography to keep Li’s scenes intact while he continued to fight with a broken wrist.
Causes of Wrist Injury
Underlying causes such as repetition, sports routines, unequal ligament, tendon, or muscle strength surrounding the joint, or weakness because of previous accidents may cause pain or damage. A wrist injury can occur when striking, falling, doing dive rolls, incorrectly performing a strike with a bent wrist, improperly performed pushups, or too many handstands.
These types of actions can overwork and inflame the tissues around the joints or cause stress fractures, especially when performing the same repetitive movement regularly. Falling onto an outstretched hand or arm, using heavy weights improperly, or throwing incorrectly may all cause wrist pain and sprains, strains, breaks, or fractures.
Wrist Injury Symptoms
An injury to the wrist may exhibit different types of pain, depending on the cause. Pain from not warming up properly may feel like a mild tweaking or aching along one side of the wrist or hand. Repetitive use may create carpal tunnel syndrome which causes a variety of symptoms, including feeling of numbness, tingling, weakness, difficulty moving, or pins-and-needles sensations, especially at night.
Types of Wrist Injuries
The wrist is very susceptible to injury in MMA. The extent of wrist injuries to MMA artists is much more than in boxers. An improper punching or fighting technique can cause injuries. Grappling and excessive joint manipulation can cause sprains and fractures in the wrist bones. Years of training can also cause degenerative changes in the wrist that puts it at further risk for injury. The following injuries are common in the wrist, Carpal tunnel syndrome, ganglion cysts, fracture of the scaphoid bone, and Kienbock's disease.
Wrist Injuries Are Very Common in Combat Arts
We Can Teach You How to Avoid These Troublesome Injuries
Related Injuries
Any MMA artist knows that for combat, the full range of motion of the wrist, fingers, and thumb is necessary. The repetitive flexion of the wrist can press on the carpal tunnel. The additional pressure compresses the median nerve. It is an entrapment neuropathy that is so common that it accounts for about 90% of all neuropathies.
Symptoms
Causes
The carpal tunnel is a very narrow passageway that connects the wrist to the hand. Tendons, ligaments, vessels, and nerves pass through it. Carpal tunnel results from a combination of compression and traction. In MMA, various moves like grappling, throwing, grabbing, increase the pressure, obstruct venous outflow, increases local edema and compromises the median nerve's intraneural microcirculation.
So nerve function is compromised. The structural integrity of the nerve is affected by repetitive insult. The myelin sheath develops lesions over time. Gradually, the surrounding tissues become inflamed. They lose their protective and supportive ability.
The repetitive traction and wrist motion in MMA exacerbate the condition and further injures the nerve. Simultaneously, if any of the nine flexor tendons that pass through the carpal tunnel are inflamed, they can compress the median nerve.
To learn how Carpal Tunnel is diagnosed Click Here
A ganglion cyst is also called a Bible cyst thanks to the many those in the combat arts who simply bang them with a Bible instead of treating it. It is considered the most common neoplasm of the hand or wrist. They result from repetitive microtrauma encountered in various martial arts involving the hands. The microtrauma then causes the degeneration of the connective tissue. They are also sometimes found in the knee and foot. Nevertheless, they are the most common soft tissue lesions in the wrist.
Symptoms
Causes
The ganglion cysts account for about 60% of all soft tissue lesions in the wrist. They are more common among female those in the combat arts. In male fighters, with repetitive wrist tension, they are common as well. Chronic microtrauma leads to the connective tissue disintegrating into mucin. Cysts grow from the mesenchymal cells at the synovial capsular junction. The persistent micro-injury to the ligaments and joint capsules stimulates the repair of the connective tissue with fibrous tissue or fibroblasts. These fibroblasts produce hyaluronic acid. This is the jelly-like mucinous material found inside the ganglion cysts. Many martial artists use their wrists to do moves. The wrist joint is involved in many techniques, throws, and maneuvers. This repeated trauma can lead to micro-tears in the joint capsule, leading to ganglion cysts. 70% of them are found on the dorsal aspect of the wrist.
To learn how is Ganglion cysts diagnosed Click here
Kienbock’s disease usually is known as lunatomalacia. It occurs due to the avascular necrosis of the lunate bone. The lunate bone is one of the many small bones of the wrist. This is a rare fracture but is common in martial arts. Many sudden forceful movements and deceleration of the wrist can fracture the lunate bone. This disrupts the blood supply causing the bone to gradually diet without blood supply.
The cause of Kienböck’s disease is multifactorial. The first cause has been identified due to shortened ulnas.
A short ulna causes excessive mechanical stress and repetitive microtrauma to the lunate bone. This is due to the relatively long radius exerting its pressure on the lunate. 78% of Kienböck fighters have these shorter ulnas.
Another cause is the loss of blood supply to the lunate bone. This bone receives blood from many dorsal penetrating arteries from the radiocarpal and intercarpal arches. The arteries of the bones in the fingers also provide blood. When blood supply via these arteries is lost due to microtrauma or macrotrauma, the bone gets necrosed. It starts dying without nutrients.
If the lunate bone is very small and has to carry a larger axial load, then the risk of developing this disease is much higher. Lunate bones can be either square or rectangular shapes. If they have a triangular shape where it has a weaker trabecular pattern Kienböck disease develops easily and progresses quicker.
Also, movements or MMA actions where the radial inclination angle decreases, can also cause the development of Kienböck’s disease. The radial inclination angle is the angle between the horizontal and a line drawn from the tip of the ulna to the tip of the radial styloid. As the angle decreases, the risk of developing Kienböck disease increases.
To learn how Kienbock's disease are diagnosed Click here
Boxer and MMA fighter Victor Ortiz shattered his wrist during the last punch of a fight. Multiple wrist bones were fractured. He was out for well over a year but continued to train with his right hand. Scaphoid fractures are common in carpal bones of those in the combat arts. They account for 60-70% of all carpal bone fractures. The problem with this injury is that it is highly deceptive. The fracture of the scaphoid is often misdiagnosed as a wrist sprain.
The scaphoid bone is the largest of the eight carpal bones in the wrist. It has a proximal and a distal portion connected by a waist. The blood supply is retrograde in the scaphoid. This means the distal portion gets blood first and then supplies the rest of the bone. During a high pressure punch, or sudden deceleration to a high-intensity wrist action or move, the waist is fractured. This disrupts the blood supply to the proximal part of the bone. Without an adequate blood supply, the bone starts to necrose and die. About 100% of all proximal fractures of the scaphoid bone develop necrosis.
To learn how Fracture of the Scaphoid are diagnosed Click here

Common Injuries
Learn more about common wrist injuries such as fractures, dislocations, and bursitis in our Common Injuries section.
Wrist Injury Diagnosis
The diagnosis of wrist injuries is remarkably diverse. A wide variety of tests are used to test, diagnose, and confirm these injuries. Apart from imaging, electromyography plays an important role in identifying whether the nerves or muscles are injured. Nerve conduction studies also confirm which part of the nerves are damaged.
Injury Specific Diagnosis
Physical Exam
On the physical exam, the doctor will observe the thumb, 2nd and 3rd digit, and the radial half of the 4th digit. They will check for the "flick sign." This is a sign where the symptoms improve when the fighter flicks their hand and wrist. The clinical physical exam also tests for sensory and motor deficits. Any evidence of thenar wasting is examined. There are several special tests specific to carpal tunnel syndrome. The best one is the carpal compression test. The doctor applies firm pressure directly over the carpal tunnel for thirty seconds. If the fighter experiences paresthesia or pain, the test is considered positive.
Phalen's test or ‘reverse prayer’ is also diagnostic. The doctor asks the fighter to fully flex their wrists. This is done by placing the dorsal surfaces of both hands for about one minute. If there is pain, it is a positive test. The reverse test is where the fighter extends both wrists by placing the palmar surfaces of both hands for 1 minute. The position looks like the fighter is praying. If there is pain, it is considered a positive test. Another test is the Hoffmann-Tinel sign. Here the doctor taps over the carpal tunnel to stimulate the median nerve. If there is pain it is considered a positive test.
Imaging
X-rays are the first test ordered to review any past injuries, arthritis, or recent trauma. Ultrasounds and MRI’s can provide a three-dimensional view of the median nerve. However, electromyography and nerve conduction studies are diagnostic for Carpal tunnel syndrome. An electromyogram studies the functioning of the nerves and muscles by measuring the electrical impulses. These impulses are evaluated along the nerves, nerve roots, and muscles. It’s done by inserting a tiny needle electrode through the skin into the muscle. The electrode measures the electric impulses generated by muscle cells as they are activated by the nerves.
Nerve conduction studies measure how fast an electric impulse is traveling through a nerve. During a nerve conduction test, the nerve is stimulated. Its response is measured. If the response is slow in an area, that part of the nerve is compressed. In carpal tunnel syndrome, the electrical response is slower in the carpal tunnel.
Lab Tests
There are no blood tests to confirm Carpal Tunnel Syndrome. It is diagnosed clinically. Doctors may request other blood tests to confirm inflammation, but this is less likely.
To learn how Carpal Tunnel is treated Click Here
Physical Exam
On physical exam, the ganglion cysts are firm, well-circumscribed, and freely mobile masses. This is important as it needs to be differentiated from a sebaceous cyst or other inflammatory cysts. They are approximately 1-3 cm in size. Very often, they are fixed to the deeper tissue and not beneath the skin. The carpal tunnel, median nerve, and flexor tendon sheath are checked to see for carpal tunnel syndrome. The muscle innervation of the ulnar nerve is confirmed, and radial pulses are examined. This is because volar wrist ganglion cysts can cause ulnar nerve neuropraxia and compress the radial artery. This can lead to wrist ischemia. Occasionally, doctors will use the transillumination test. Here the doctor will dim the lights and use a bright light to illuminate the cyst and see if it is clear or contains material. Ganglion cysts usually transilluminate in this test.
Imaging
Plain films are ordered to rule out intraosseous causes. For ganglion cysts, radiographs are unremarkable. If the doctor wants to rule out a solid tumor, MRI is indicated. The MRI will show a well-circumscribed area. Ultrasound is also helpful, as it differentiates a cyst from a vascular lesion. This can be potentially dangerous if the cyst is biopsied. The puncture of the radial artery in a vascular lesion via needle aspiration can lead to profuse bleeding.
Lab Tests
There are no blood tests to confirm ganglion cysts. Imaging is mostly diagnostic and blood tests are only required if surgical intervention is recommended.
To learn how is Ganglion cysts treated Click here
On physical examination, doctors will check for wrist swelling and tenderness over the lunate. They will examine the nerves and muscles in the area. A thorough musculoskeletal exam and neurological exam is done to confirm synovitis and any loss of grip strength. Wrist range of motion exams is performed.
Kienböck disease is both a clinical and imaging diagnosis. For imaging, CT and MRI are highly specific. However, MRI is the most sensitive and can pick up occult cases that are easily missed on plain film and X-Ray. MRI images vary with the extent of osteonecrosis and how far it has progressed. It’s helpful because it can also demonstrate the integrity of the articulating cartilage.
Plain films can miss the disease especially early on because there is no diffuse lunate sclerosis. Cystic changes are absent and articular surfaces have not yet collapsed. There is no carpal collapse, mid-carpal, and radio-carpal in the early stages. To aid surgical planning, CT is sensitive. It can detect subtle subchondral fractures, coronal lunate fractures if present, any fragmentation, carpal instability in the fingers, and the degree of trabecular disruption.
Nuclear Scintigraphy was an adjunct for diagnosing early disease. Since it’s non-specific, it’s been replaced by the MRI. It uses tracers of radioactive molecules to diagnose diseases captured by gamma rays.
Staging is very important for this disease because it influences what treatment and the prognosis of the injury.
The Lichtman Classification is used, based on radiographic and MRI imaging.
Stage 1: Normal Xray, lunate intensity changes on MRI.
Stage 2: Lunate sclerosis on Xray with or without fracture. The lunate bone has a normal shape.
Stage 3: Collapse of the lunate articulating surface.
A: with preserved carpal alignment and height.
B: with scaphoid flexion and loss of carpal height.
C: with associated coronal fracture
Stage 4: Stage 3B + radio-carpal or mid-carpal arthrosis.
Functional Staging uses contrast-enhanced MRI to assess bone perfusion and the extent of necrosis. It is done to guide surgical techniques to revascularize the bone.
Stage 1: Bone marrow ischemia and edema but a viable lunate
Stage 2: Partial necrosis. The viable portion of bone is usually distal
Stage 3: Complete necrosis
Kienböck disease does not need to be confirmed with blood tests. The disease is diagnosed and staged with the help of imaging. Blood tests are only required for surgical treatment as part of the pre-operative clearance.
To learn how Kienbock's disease are diagnosed Click here
The physical examination of the wrist usually uses the “look, feel, move” pattern. Doctors will first look for a deformity. Deformities are usually not visible in scaphoid fractures unless there are other associated carpal fractures. They will palpate the distal radius and ulna and metacarpals. This is to assess associated injuries and fractures. The classic sign is tenderness in the anatomic snuffbox.
This snuffbox is located between the first and third extensor compartments. Two muscles lie radially; abductor pollicis longus and extensor pollicis brevis. On the ulnar side, lies the extensor pollicis longus. Some tenderness is observed directly over the scaphoid tubercle. This is not always the case. The scaphoid tubercle is felt as a bony prominence at the level of the distal palmar crease.
Tenderness found in one of the three locations is clinically diagnostic:
Another more sensitive test is the scaphoid compression test. Here the doctor places the examining index finger and thumb over both poles of the scaphoid and compresses. If a fracture exists, then it will elicit pain. Typically, any pain in the anatomical snuffbox on the ulnar deviation of the wrist is suggestive of a scaphoid fracture.
Plain films are the first step in imaging the scaphoid fractures. AP and lateral views are taken. A special scaphoid view where the wrist is extended at 30⁰ and 20⁰ of ulnar deviation is done. Scaphoid fractures are easily missed on plain film. Up to 25% of scaphoid fractures are not visible on initial X-rays. Doctors might immobilize the wrist in a splint or cast for 1-2 weeks and repeat the Xray. For many fighters, bone scans are done to diagnose occult fractures 72 hours after the initial injury.
If symptoms persist and X-rays are clear MRI or CT is done. MRI is the most sensitive. It can also identify any injury to the ligaments or bone edema. CT scan is also fairly accurate but can miss fractures with less than 1 mm displacement.
There are no special laboratory tests unless surgery is to be done. For preoperative clearance, the routine blood tests, including full blood count, urea, and electrolytes, clotting screen and group and typing, are done.
To learn how Fracture of the Scaphoid are treated Click here



Common Diagnoses
Refer to our Common Diagnoses section to learn more about how injuries affecting the many ligaments and bones in the wrist joint are diagnosed.
Wrist Injury Treatment
The treatment of wrist injuries is diverse. It depends on the stage of diagnosis; early vs late. It also depends on the type of injury. Injuries due to fractures need to be surgically treated while conservative treatment suffices for Carpal Tunnel Syndrome.
Injury Specific Treatment
Emergency Treatment
Carpal tunnel syndrome is rarely an emergency as it develops over time. If there is a sudden exacerbation of pain and other symptoms, then symptomatic treatment is advised.
Medical Treatment
Conservative treatment is recommended for all fighters if carpal tunnel syndrome is identified early. The first step in treatment is to modify wrist activities that increase pressure in the carpal tunnel. Minimize repetitive flexion, extension, abduction, and adduction. For fighters who are bulkier, some weight loss can help. Combined therapy with wrists splints and physical therapy is better than single treatment alone. Pain medications like nonsteroidal anti-inflammatory drugs relieve pain. Though this is just a temporary solution.
Occasionally, if conservative treatments fail, steroids are the next option. An oral glucocorticoid can also provide relief. In cases of persistent carpal tunnel syndrome, surgery with carpal tunnel release is done. This procedure is done after nerve conduction studies show substantial axonal degeneration. This procedure is considered minor and can be done endoscopically. The transverse carpal ligament or flexor retinaculum is incised, allowing more space in the carpal tunnel. This eases the pressure on the median nerve. The surgery is typically a day procedure.
Home Treatment
Night wrist splints are recommended. Occupational hand therapy is beneficial. Many wrist issues may be helped by certain hand exercises or movements found in martial arts such as tai chi. See Fighting Arts article on “Body Strengthening Methods.”
Emergency Treatment
Ganglion cysts are usually not medical emergencies given that they take place over time and continuous micro-trauma. Asymptomatic lesions can be left as they are. Lesions that cause severe pain, weakness, or neuropathies must be treated.
Medical Treatment
Fighters who are asymptomatic can be observed. Many ganglion cysts spontaneously regress. Treatment also depends on the location of the cyst. Dorsal wrist ganglion cysts are aspirated. That is a procedure where the fluid is drained from the cyst with a syringe. With aspiration, ganglion cysts tend to recur and so surgery is preferred.
Volar wrist ganglion cysts are not aspirated since they lie very close to the radial artery. The chances of bleeding are very high. Surgery is better for them and also for those fighters who are symptomatic. It’s also preferred in whom conservative treatment has failed. During surgery, the cyst is excised. An incision is usually made directly over the cyst. It is carefully dissected to expose the pedicle of the cyst. The capsule and all its attachments are removed to prevent any recurrence.
Home Treatment
Despite surgical excision, ganglion cysts have a high recurrence rate. Avoiding repetitive wrist motions for 6 weeks can help. Warm compresses improve circulation. Wrist braces and splints are also helpful.
If Kienbock's disease is suspected, then pain relief and immobilization is the first step. Seek a referral to an orthopedic doctor.
The goal of treatment in Kienböck disease is to relieve pain, preserve wrist motion, and preserve grip strength.
The treatment as mentioned earlier depends on the stage and the cause.
Stage I is always treated with splints or immobilization via the cast.
Stage II is also treated with immobilization if the bone is not completely necrosed.
Stages II with complete necrosis, III, and IV require surgery. It’s called "joint-leveling" surgery. Occasionally, it is done with bone grafting or transfer of arterial branches from adjacent vessels.
Stages with lunate collapse and wrist degenerative changes may need more surgery like proximal row carpectomy. For those with shortened ulnas, the most common procedure to relieve the lunate is radial shortening osteotomy.
Following surgery, six to eight weeks of rest is needed. No immediate return to repetitive and wrist action is permitted.
Following any trauma to the wrist, if a scaphoid fracture is suspected, imaging must be done immediately. In suspected fractures with positive clinical signs on examination but no radiographic proof, imaging must be repeated in a week after splinting. If the pain persists and X-rays are still normal, then MRI or CT is advised. Immobilization with pain relief is advised.
The non-operative management or conservative treatment is advised for non-displaced fractures. It is also recommended for fractures within the distal third of the bone. The wrist is immobilized either with a long or short arm cast and with or without thumb spica to immobilize the thumb. The cast is kept for six weeks. X-rays are done after this to ensure the union of both parts of the scaphoid bone. The location of the fracture determines the time it takes to heal. Fractures in the distal-third heal within 6-8 weeks. Fractures in the middle-third heal in 8-12 weeks. Fractures in the proximal third take the longest; 12-24 weeks.
Surgical fixation is done when the displacement if more than 1mm, there’s a humpback deformity, the radiolunate angle is more than 15,transcaphoid perilunate dislocation, comminuted fractures, fractures in the proximal pole, non-displaced waist fractures in those in the combat arts who use wrist maneuvers, and those with nonunion or avascular necrosis after conservative treatment has failed.
During surgery, single or multiple screws are inserted. The procedure is done percutaneously or via open surgery. Open surgery is recommended for non-unions and large displacement. Percutaneous surgery is for acute, minimally displaced fractures.
For those fighters who continue to have nonunion, open reduction and internal fixation with bone graft are recommended. A bone graft is taken from the distal radius or the iliac crest.
Alternative treatments are salvage procedures, like excising the proximal fragment, total or partial fusion, radial styloidectomy, or proximal row carpectomy.
Immobilization is important as the scaphoid bone takes very long to heal. Any repeat injury can cause the bone to necrose forever as it fails to unite. Pain relief can be achieved with NSAIDs. Repeat X-rays at regular intervals are necessary to ensure the bone is healing.



Common Treatments
Learn more about how healthcare professionals treat injuries using physical therapy, medications, surgery, and other approaches in our Common Treatments section.

