Combat Arts Thigh Injuries Overview

Leg kicks and oblique kicks in MMA can be powerful. They pack a punch. Josh Emmet suffered a knee injury in the early rounds against Shane Burgos. The ACL tear was just one of the injuries he suffered. He also had an impact fracture of the femur and it has put him on a long road to rehab. He refuses to quit.
Thigh muscles consist of hamstrings in back, adductors on the inside, and quadriceps muscle in the front of the leg. They are responsible for hip flexion and are the primary muscles utilized for balance and locomotion. Thigh injuries occur when one or more muscles in the front of the thigh have been strained or torn.
Thigh Injury Causes
Thigh muscles consist of hamstrings in back, adductors on the inside, and quadriceps muscle in the front of the leg. They are responsible for hip flexion and are the primary muscles utilized for balance and locomotion. Thigh injuries occur when one or more muscles in the front of the thigh have been strained or torn.
Chronic hamstring injuries occur because a prior injury was improperly rehabilitated and small amounts of trauma are repeated over a long period (i.e., kicking or leg locks). Poor hamstring flexibility increases the likelihood of small tears, which can cause the muscle to shorten and get tighter. A vicious circle is then established.
Thigh Injury Symptoms

Types of Thigh Injuries
Thigh injuries form about 3.6% of MMA injuries in athletes. Other than muscle contusions and lacerations, the most important injury in the thigh is that to the femur. The femur is one of the strongest and longest bones in the body.
Related Injuries
Femoral Fractures
Fractures of the femur can be life-threatening. High energy trauma can affect the neck and shaft of the femur. Powerful kicks to the thigh area can damage the bone. Stress fractures can also develop due to repetitive trauma and strain on the thigh. The femur is surrounded by three large muscle compartments that are susceptible to injury and hemorrhage.

Moreover, any injury to the femur could damage the sciatic nerve which lies very close to the bone. The femoral artery is also vulnerable to injury. This is a large artery that supplies the lower leg. The risk of bleeding and shock due to an injury to this artery is very high. Since the femur is a large bone, there is also the risk of fat embolism as fat from the bone marrow leaks into the systemic circulation. Therefore, mortality rates in femoral fractures are very high and those who are injured by them need to be watched closely.
Femoral Fractures Causes
In combat sports, repetitive oblique kicks can cause stress fractures in the femoral neck and shaft. Acute injuries due to violent high-intensity punches, kicks, and sudden falls. Outside leg kicks with massive torque can injure the muscles and disrupt the bone. Similarly, high kicks with a full power leg can cause the neck of the femur to fracture.
Femoral Fractures Symptoms

To learn how Femoral Fractures is diagnosed Click Here.
Common Injuries
Learn more about common thigh injuries such as lacerations and muscle in our Common Injuries section.
Thigh Injury Diagnosis
To diagnose injuries in the thigh, the physical exam is important, but imaging is the key. This includes multiple modalities including plain films, CT, and MRI to evaluate the muscle compartments in the thigh. Moreover, since the femoral artery could be injured, to prevent hemodynamic compromise blood tests are also necessary to understand the extent of the damage.
Want to Know What to Expect When a Physician Diagnoses a Thigh Injury?
Get Our Free Newsletter to Get the Latest Injury Management Information.
Injury Specific Diagnosis
Femoral Fractures
Physical Exam
In trauma to the femur, the physical exam is done very quickly. The range of motion exercises of the hip and knee are done to rule out any injury to these joints. A very thorough neurovascular examination is done. Those with displaced fractures have a shortened and externally rotated lower limb. The ATLS (Adult Trauma Life Support) protocol is indicated for femoral fractures and so vitals signs are assessed and closely monitored. In the case of a fall, the ankle is also examined.

Imaging
Plain films must include the following views: anterior-posterior (AP) pelvis, AP and lateral hip, AP and lateral femur, AP and lateral knee. All bones and joints related to the thigh have to be assessed. The CT scan classifies the pattern of the fracture and can even visualize a subtle fracture line. It can also display and evaluate the femoral neck.
MRI is not used in an acute injury. For femoral neck stress fractures, they are better than the CT.
A chest radiograph and electrocardiogram (EKG) are necessary to evaluate the lungs and heart. This is to watch out for any signs of fat embolism and hemodynamic compromise.
A femoral neck fracture is classified by Garden and Pauwel classifications as follows
The Garden Classification:
Type I: Incomplete fracture - non displaced
Type II: Complete fracture - nondisplaced
Type III: Complete fracture - partial displaced
Type IV: Complete fracture - fully displaced
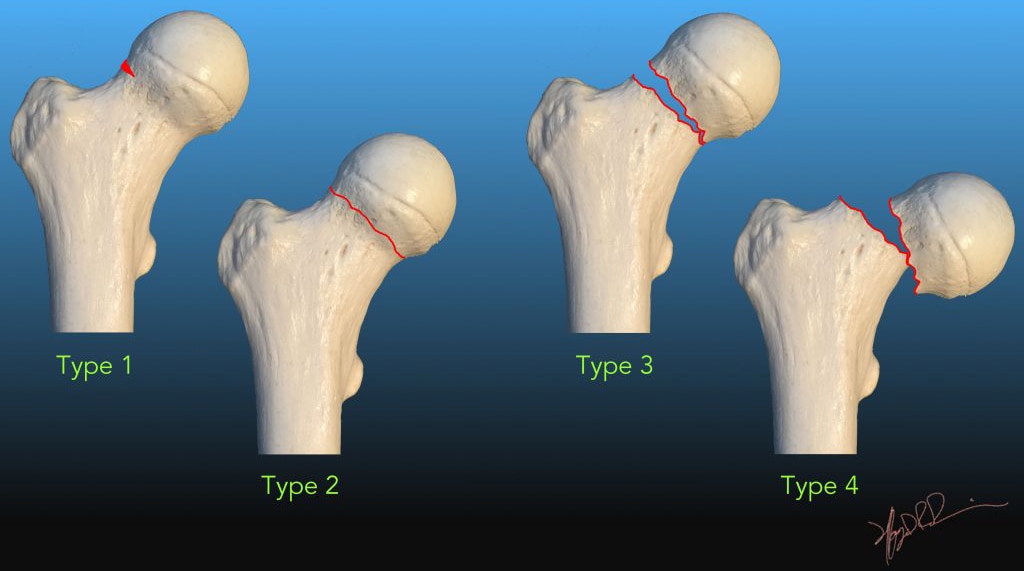
Source: faculty.washington.edu
The type of fracture determines the treatment.
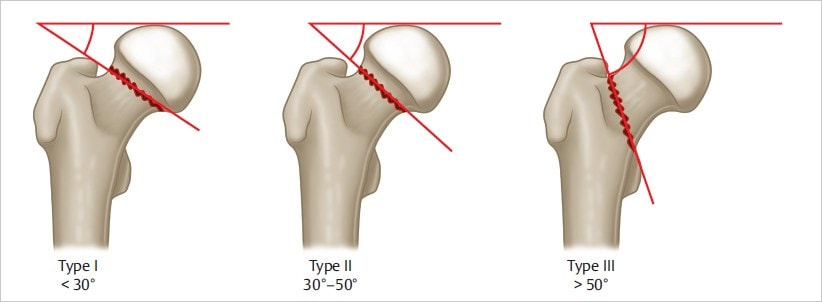
Pauwel Classification:
Type I: < 30 degrees
Type II: 30-50 degrees
Type III: > 50 degrees
Classification of femoral shaft fractures by the AO/Orthopaedic Trauma Association classification. It classifies the fracture type resulting in 27 different patterns.
32A – Simple
A1 – Spiral
A2 – Oblique, angle > 30 degrees
A3 – Transverse, angle < 30 degrees
32B – Wedge
B1 – Spiral wedge
B2 – Bending wedge
B3 – Fragmented wedge
32C – Complex
C1 – Spiral
C2 – Segmental
C3 – Irregular
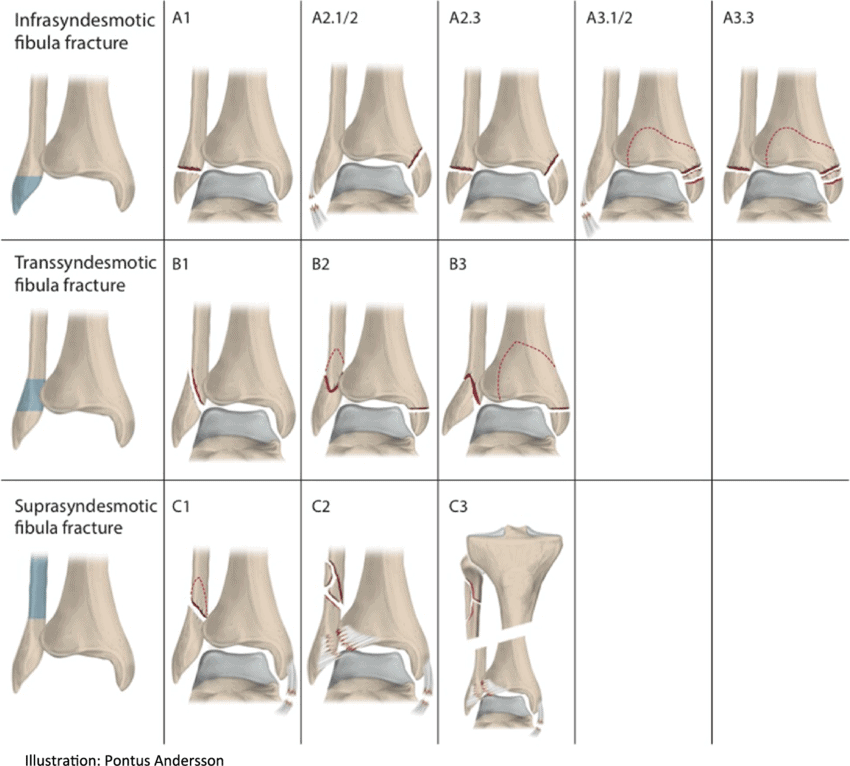
Source: BMC Musculoskeletal Disorders
Lab Tests
Blood tests are done to assess hemodynamic status. This includes complete blood, count, basic metabolic panel, Rh, and typing for a cross match. In preparation for surgery, other blood tests like a coagulation profile might also be done.
To learn how Femoral Fractures is treated Click Here
Common Diagnoses
Learn more about how physicians use a variety of tests to diagnose injuries in the thigh in our Common Diagnoses section.
Thigh Injury Treatment
Femoral neck and shaft fractures are almost always treated surgically especially in the acute setting. However, there is a high mortality rate for this injury, about 20-30% within the first six months. Therefore, all femoral fractures need to be treated promptly.
Injury Specific Treatment
Femoral Fractures
Emergency Treatment
ATLS protocol is activated since the thigh can hold around 1.5 L of blood. Any vascular injury can contribute significantly to shock. Intravenous fluids and cardiac monitoring are essential.
Medical Treatment
Treatment of femoral shaft fractures can be medical or surgical. The most common treatment for those in combat sports is intramedullary nailing. Other operative techniques include plate osteosynthesis and external fixation.

In some cases, closed treatment with traction, splinting, and casting is tried temporarily.
Intramedullary Nailing is done in stable athletes within 24 to 48 hours. It allows early weight-bearing and is therefore preferred.
Antegrade Nailing is done if the treatment proceeds in the first 24 hours after surgery.
Retrograde Nailing is done if there are associated femoral neck and tibial fractures.
Reaming is a technique of preparing the medullary canal using a surgical reamer.
Plate Osteosynthesis is done via Open reduction internal fixation (ORIF) techniques. ORIF is typically not used as a primary treatment of femoral shaft fractures. It is done when IM nail fixation is contraindicated.
Minimally invasive techniques such as minimally invasive plate osteosynthesis (MIPO) does not expose the fracture site and bridge plating can be done instead.
External Fixation is done for everyone with an open fracture, in those who are unstable and with extensive vascular injury.
Traction can serve as a temporary measure. The following traction devices are used: Thomas, Hare, Sager, Kendrick, CT-6, Donway, and Slishman splints for apparent femoral injuries. Longitudinal traction can stabilize the fracture site, gross length, alignment, and rotation. It can relieve pressure on the nerves and blood vessels. It can restrict bleeding by stabilizing the surrounding clot. They are switched for fiberglass or plaster splint or skin vs. skeletal traction in the hospital.
Skin traction or Bucks traction is applied via a boot attached to a counterweight.
In skeletal traction, a pin is placed through the bone to prevent the soft tissues from bearing the traction force. Pins are usually placed in the distal femur, proximal tibia, and calcaneus.
Home Treatment
After surgery, the hospital stay is long. To prevent systemic complications, serial blood tests are required to assess anemia, renal insufficiency, and other metabolic disorders. Fighters thigh area has to be checked daily for compartment syndrome, wound healing, and neurovascular compromise.
After surgery, physical and occupational therapy begins in the hospital itself. They are important to regain mobility and function. At home, these exercises must continue. Weight-bearing is permitted as tolerated.
Driving is only allowed when a person can bear weight and break safely without any pain. Smoking is not permitted.
Common Treatments
Our Common Treatments section discusses the various treatments for injuries to the thigh.

